An unforeseen benefit to California’s physician-assisted death law
Originally published in the LA Times August 21st, 2017. Article archived below.
Some doctors in California felt uncomfortable last year when a new law began allowing terminally ill patients to request lethal medicines, saying their careers had been dedicated to saving lives, not ending them.
Many healthcare systems designed protocols for screening people who say they’re interested in physician-assisted death, including some that were meant to dissuade patients from taking up the option.
But physicians across the state say the conversations that health workers are having with patients are leading to patients’ fears and needs around dying being addressed better than ever before. They say the law has improved medical care for sick patients, even those who don’t take advantage of it.
“One doctor said we should be able to order the End of Life Option Act without the drugs,” said Dr. Neil Wenger, director of the UCLA Health Ethics Center. “It really has created a new standard for how we ought to be helping people at the end of life.”
California last year became the fifth state to allow people with terminal illnesses to request pills from their doctors to end their lives. In the first six months the law was in effect, 111 terminally ill patients ended their lives that way, state officials said.
The law requires that two doctors agree that the patient has an incurable illness with no more than six months to live and has the mental capacity to make such a decision. Many health systems set up additional protocols for patients who express interest in the law.
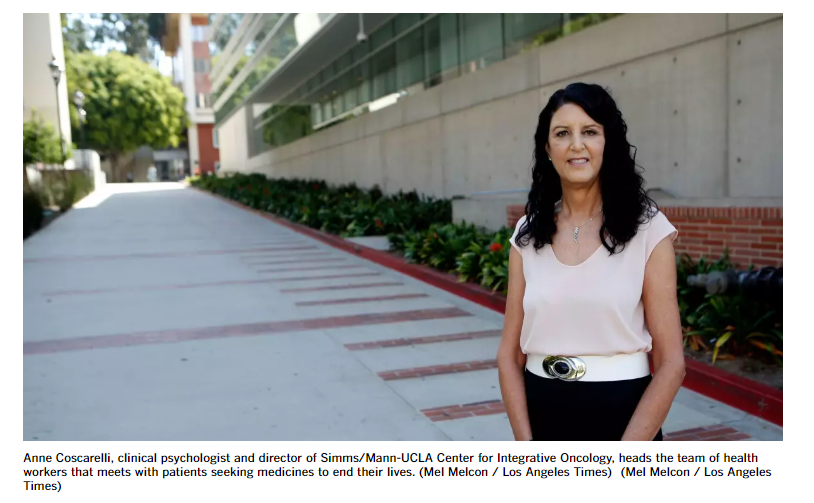
At UCLA, they’re required to talk to psychologists or social workers, which often reveals concerns that weren’t being addressed, said Anne Coscarelli, a clinical psychologist who heads the team of health workers that meets with these patients.
The health workers ask patients a variety of questions: what scares them, how they’re feeling, what they’re worried about, what defines their quality of life.
Sometimes doctors end up adjusting patients’ medicines or treatments because patients hadn’t before expressed how much pain they were in. Some patients decide to go on hospice earlier than they would have otherwise.
“Not everyone who’s talking about this is saying, ‘I want this medication.’ They’re saying, ‘I’m suffering’ or ‘I’m worried about suffering’ and that becomes the conversation starter ... and it might not come up in any other way,” Coscarelli said.
First 6 months of aid-in-dying in California
191 people prescribed lethal medications
111 died from taking lethal medications
Of the 111, 87% were at least 60 years old
96% had health insurance
84% were receiving hospice or palliative care
59% had cancer
Sources: California Department of Public Health
Approximately 100 patients at UCLA began the process to receive a prescription in the first 12 months the law was in effect, but only about a quarter ended up getting prescriptions, Wenger said.
Coscarelli said psychologists and social workers have also helped patients come to terms with dying. For some, it can be as simple as getting their legal or financial affairs in order.
Others have confronted the question of what legacy they will leave behind. Some record video messages for their loved ones. One woman put together a folder for each of her children and grandchildren filled with stories about them and stories about her, Coscarelli said.
“That becomes something that we can introduce people to in these conversations, whereas they might not have ever thought about it,” she said.
Doctors have sometimes struggled to talk about dying with patients. According to a 2015 Kaiser Family Foundation survey, 89% people believe doctors should discuss end-of-life care with patients, but only 17% had had such a conversation with their health care provider.
But now, physicians say patients are curious about the law and asking about it, which provides them an opportunity to have these frank discussions.
A study from Oregon, which legalized aid-in-dying 20 years ago, found that though only 1 of 640 terminally ill patients took lethal medications, 1 of 50 talked to their physician about it and and 1 in 6 talked to their families about it.
“There’s a lot of need for talk, and talk is something that’s bigger and broader than the actual aid-in-dying itself,” Coscarelli said.
Dr. Bob Uslander, who specializes in palliative and hospice care, said that at a recent speaking event in San Diego, he fielded dozens of questions about not just physician-assisted death but also other end-of-life care options.
He said he thinks the unprecedented interest spurred by the law will lead to more thoughtful planning around death, such as the creation of more advanced care directives.
“We’ll get more people to actually make their wishes known and document their wishes,” Uslander said.
The law still faces heavy opposition from some corners. Many doctors still don’t want to write the prescriptions. A group of doctors has also filed a lawsuit saying that the law essentially decriminalizes assisted suicide and strips terminally ill patients of their protections under state law. A judge ruled earlier this summer that the case would be allowed to go to trial.
Doctors aren’t required to participate in the law and health systems can opt out. At Catholic and church-affiliated hospitals, which make up 13% of all acute care hospitals in the state, doctors are not allowed to prescribe such medications.
But even at those institutions, requests for the medicines have sometimes helped identify issues that health workers can assist with, said Lori Dangberg, vice president of the Alliance of Catholic Health Care. Patients fear they’ll be a burden on their families, or are scared of what’s to come, she said.
The Catholic and church-affiliated hospitals have also begun a collaboration with local dioceses to hold workshops on end-of-life matters, she said. The Archdiocese of Los Angeles now offers a workshop on end-of-life care including ethics, palliative and hospice care as well as pastoral care at the end of life.
“I think what this new law has done, it’s really a reminder we need to do a much better job with caring for people through the end of life,” Dangberg said.
Dr. Stephen Lockhart, chief medical officer for Sutter Health, said that before the law went into effect, doctors received training in how to talk about aid in dying, but also in other end-of-life options. They had their questions answered by medical ethicists.
He said that more patients are broaching the topic with their physicians than before. Even patients who have wills or advanced care directives had not always planned out their end-of-life wishes with their families.
“It takes a certain amount of courage to step into those conversations and ... we have people now stepping into those conversations and they now have the support to move through them,” he said.